
Hemocompatibility
Blood compatibility-ISO 10993-4, GB/T 16886.4,GB/T14233.2, ASTM F756,ASTM F2382, ASTM F2888, refers to the desired response of blood to an exogenous substance or material. Generally refers to the compatibility between the material and the various components of the blood.


Introduction of Blood Compatibility Test
Blood compatibility refers to the desired response of blood to an exogenous substance or material. Generally refers to the compatibility between the material and the various components of the blood.
Application of standard
ISO 10993-4, GB/T 16886.4,GB/T14233.2, ASTM F756,ASTM F2382, ASTM F2888
Test Method and Principle
Thrombosis |
The internal phenomenon of partial or complete occlusion of blood vessels and instruments caused by thrombus. In many cases, the thrombosis test combines the test principles of blood coagulation, platelet, hematology, and complement system. |
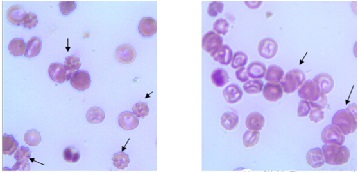
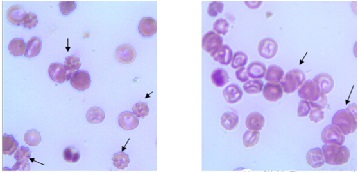
In Vitro Hemolytic Test |
Hemolysis is the release of hemoglobin from the red blood cell due to rupture or through a partially damaged but intact cell membrane. Hemolysis test is to observe whether the test material causes hemolysis or erythrocyte coagulation and other reactions. The sample and controls are contacted with fresh diluted rabbit blood, and the absorbance at 540nm/545nm is determined by spectrophotometer. |
Coagulation Test (PTT) |
The test involves screening for the ability of circulating blood to contact the device material to induce clotting through internal clotting pathways. Partial determination of thromboplastin time (PTT) - a test that improves activated partial thromboplastin time (APTT). Unlike the APTT test, PTT analysis uses reagents (rabbit encephalin) that do not contain activated substances such as silica, kaolin, or elastic acid. The material under test acts as an activator. The purpose of this test method is to determine the time it takes for citric acid plasma exposed to medical materials to form blood clots when exposed to phospholipid particles and calcium chloride suspension. |
Hematology |
Flow cytometry can be used to evaluate the imbalance of white blood cell count. The increase of reticulocyte count indicates the proliferation of red blood cells in bone storage. Elevated reticulocyte count may be caused by prolonged blood loss (bleeding), hemolysis, or other causes of decreased red blood cell mass. |
Platelet count |
Platelet count refers to the number of platelets per unit volume of blood. Platelets are the smallest cells in the blood and protect the integrity of capillaries. Since platelets play a key role in preventing bleeding, the measurement of platelet count is important. The significant decrease in platelet count in the blood after contact with the device is caused by platelet adsorption, aggregation, absorption (as in the spleen) or coagulation of the blood on the material and device. The decreased platelet count during the use of implant devices may be due to the accelerated destruction or elimination of platelets in the circulation. |
Determination of complement |
Complement (C) is a group of proteins with enzymatic activity that are present in serum and tissue fluid of human and animal after activation. As early as the end of the 19th century, Bordet confirmed that fresh blood contains a heat-resistant component, which can assist and supplement specific antibodies, and mediate immune bacteriolysis and hemolysis, so it is called complement. Complement system is a multicomponent subsystem composed of more than 30 soluble proteins, membrane-binding proteins and complement receptors, so it is called complement system. According to their biological functions, complement system components can be divided into complement intrinsic components, complement regulatory components and complement receptor (CR). An increase in any of these complement components indicates activation of the complement system. CH50 is usually referred to as CP-CH50 (classical pathway). A decrease in CH50 indicates total complement consumption. Some materials activate complement components, which in turn activate white blood cells, causing them to aggregate and be cleared in the lungs. Another in vitro method of complement activation is the formation of complement C3 invertase or C5 invertase by enzymolysis conversion. |
Period
The test period is shown in Table 1.
Test project | Test cycle |
In vivo/in vivo thrombosis test | 8 weeks |
In Vitro Hemolytic Test | 2~4 weeks |
Coagulation tests(PTT) | 4~6 weeks |
Hematological test (red blood cell, white blood cell count) | 4~6 weeks |
Platelet count | 4~6 weeks |
Complement activation test | 4~6 weeks |
Sample Request
Test project | The sample thickness(<0.5 mm) | The sample thickness(>0.5 mm) | weight |
In vivo/in vivo thrombosis test | 4(Intravenous Implantation Sample) | 15 cm2 | 1g |
In Vitro Hemolytic Test | 3 | 3*60 cm2 | 3*5g |
In Vitro Hemolytic Test-ASTM | 6 | 6*42 cm2 | 6*1.4g |
Coagulation tests(PTT) | 3 | A single sample exceeding 1g or 750px2 needs to prepare small samples of 150px2 with the same process. | |
Hematological test (red blood cell, white blood cell count) | 3 | ||
Platelet count | 3 | ||
Complement activation test | 3 | ||
Copyright © EPINTEK GROUP
Powerd by PEERHI
EPINTEK GROUP
Tel: +86 21 54736833
Address: 4th Floor, T2 Wanjin Center, Lane 360, Xinlong Road, Minhang District, Shanghai
E-mail: stefanie.sun@epintek.com




We Focus on the Demand for Innovation
